Your body has an internal clock that helps regulate daily activities like sleep and wakefulness. This natural cycle, known as the circadian rhythm, plays a key role in maintaining overall health. When it’s disrupted, it can lead to various sleep disorders, including obstructive sleep apnea (OSA).
OSA is a chronic condition where breathing repeatedly stops and starts during sleep. This can cause hypoxia, a lack of oxygen that further disrupts the body’s internal clock. Key proteins like PER, CLOCK, and BMAL1 help keep this clock running smoothly. However, in OSA, these molecular feedback loops can become unbalanced.
Understanding the connection between the circadian clock and OSA is essential. It not only sheds light on the condition but also highlights the importance of maintaining a healthy sleep cycle. Let’s explore how these factors interact and what it means for your health.
Understanding the Basics of Circadian Rhythms and Sleep Apnea
Internal clock genes help maintain daily biological processes. These genes, such as CLOCK and BMAL1, work together to keep our body’s internal clock running smoothly. They regulate everything from hormone release to energy levels, ensuring our systems function in harmony.
The central clock, located in the brain’s suprachiasmatic nucleus (SCN), acts as the master regulator. It syncs with external cues like light and darkness to keep our daily rhythms on track. When this system is disrupted, it can lead to health issues, including sleep disorders.
Obstructive sleep is a common condition where breathing pauses during rest. These episodes often occur at specific times, suggesting a link to the body’s internal clock. Understanding this connection can help in managing the condition more effectively.
Here’s how clock genes function in the body:
- CLOCK and BMAL1: These genes activate other proteins that regulate daily cycles.
- PER and CRY: These proteins provide feedback to control the clock’s timing.
- SCN: The brain’s central clock coordinates these processes.
By studying these mechanisms, researchers gain insights into how sleep apnea episodes align with circadian timing. This knowledge opens doors to better treatments and improved sleep health.
Exploring Obstructive Sleep Apnea: Symptoms and Diagnosis
Obstructive sleep apnea (OSA) is a condition that affects millions, often disrupting daily life. It’s characterized by repeated pauses in breathing during rest, leading to fragmented sleep and other health concerns. Recognizing the signs early can make a significant difference in managing the condition effectively.
Recognizing Common Signs
One of the most noticeable symptoms of OSA is loud snoring. However, it’s not just the noise—frequent awakenings and gasping for air are also common. Sleep fragmentation, where rest is repeatedly interrupted, can leave individuals feeling exhausted despite a full night’s sleep.
Other signs include morning headaches, difficulty concentrating, and irritability. These symptoms often overlap with other conditions, making it essential to seek a professional diagnosis. For example, a patient might attribute their fatigue to stress, not realizing it’s linked to OSA.
Diagnostic Methods and Tools
Accurate diagnosis is key to managing OSA. Polysomnography (PSG), an overnight sleep study, is the gold standard. It monitors brain activity, eye movement, and breathing patterns to identify disruptions. Home sleep tests are also available, offering a more convenient option for some patients.
Recent advancements in diagnostic tools have made it easier to detect OSA early. For instance, wearable devices now track sleep patterns, providing valuable data for healthcare providers. These innovations are helping to bridge the gap between symptoms and diagnosis.
| Diagnostic Method | Description | Relevance to Circadian Rhythms |
|---|---|---|
| Polysomnography (PSG) | Overnight study monitoring sleep stages and breathing. | Identifies disruptions linked to circadian rhythm misalignment. |
| Home Sleep Test | Portable device tracking breathing and oxygen levels. | Helps assess how circadian clock genes influence sleep patterns. |
| Wearable Devices | Monitors sleep duration and quality over time. | Provides insights into circadian rhythm disruptions. |
Understanding the connection between OSA and internal clock disruptions is crucial. Misaligned circadian rhythms can worsen symptoms, making timely diagnosis even more important. By leveraging modern tools and techniques, healthcare providers can offer more personalized and effective treatments.
The Science of Clock Genes and Gene Expression
The intricate dance of clock genes shapes our daily biological rhythms. These genes, including BMAL1, CLOCK, and PER, work together to regulate sleep and wakefulness. Their interactions create a feedback loop that keeps our internal timing system running smoothly.
Roles of BMAL1, CLOCK, and PER
BMAL1 and CLOCK are key players in the clock gene network. They activate other proteins that control daily cycles. PER, on the other hand, provides feedback to fine-tune the timing. Together, these genes ensure our body’s internal clock stays in sync with external cues like light and darkness.
Disruptions in these genes can lead to sleep fragmentation. This is when sleep is repeatedly interrupted, leaving individuals feeling tired even after a full night’s rest. Understanding these mechanisms helps researchers develop better treatments for sleep disorders.
How Gene Expression Influences Sleep Patterns
Gene expression is the process by which information from a gene is used to create functional proteins. In the context of sleep, fluctuations in gene expression can directly affect sleep quality. For example, when BMAL1 and CLOCK are active, they promote wakefulness. When PER is active, it signals the body to prepare for rest.
Molecular studies have shown that disrupted gene expression can lead to misaligned sleep patterns. This misalignment often results in sleep fragmentation, a common issue in many sleep disorders. By studying these processes, scientists gain valuable insights into how to improve sleep health.
| Clock Gene | Role | Effect on Sleep |
|---|---|---|
| BMAL1 | Activates other proteins | Promotes wakefulness |
| CLOCK | Works with BMAL1 | Regulates daily cycles |
| PER | Provides feedback | Signals rest |
By understanding the science behind clock genes and gene expression, we can better appreciate the complexity of our sleep patterns. This knowledge opens the door to innovative treatments and healthier sleep habits.
Mechanisms of Circadian Clock Disruption in OSA
The body’s internal timing system relies on precise molecular interactions to function properly. In obstructive sleep apnea (OSA), these interactions can be thrown off balance, leading to disrupted rhythms. One key factor is intermittent hypoxia, a condition where oxygen levels drop repeatedly during rest.
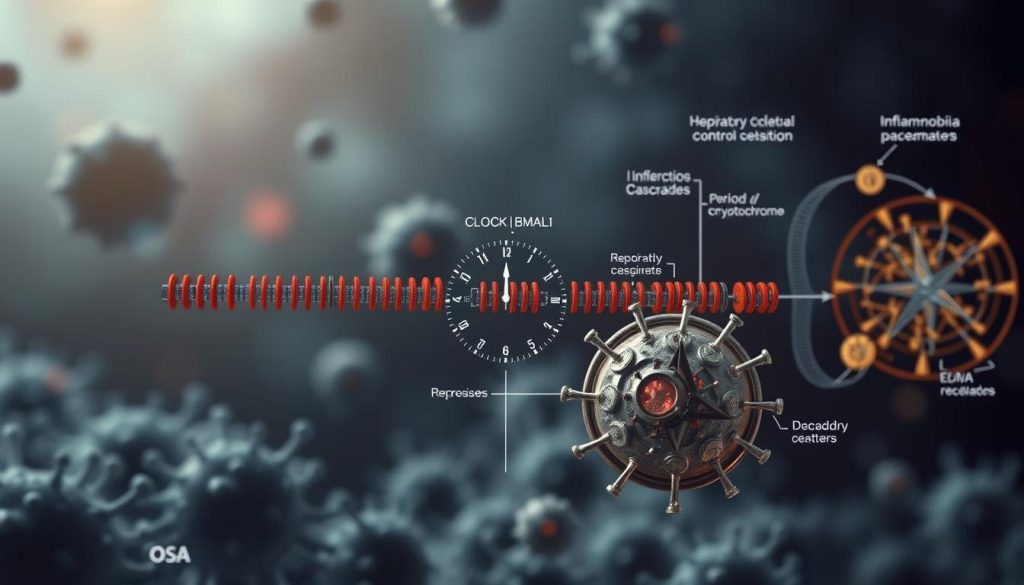
Molecular Interactions and Feedback Loops
Intermittent hypoxia affects the feedback loops that regulate the body’s internal clock. Key proteins like HIF-1 interact with clock genes such as BMAL1 and CLOCK. These interactions are essential for maintaining daily rhythms. When hypoxia occurs, it disrupts these feedback loops, leading to misaligned timing.
Research studies have shown how these disruptions play out in OSA patients. For example, altered feedback loops can lead to fragmented rest and irregular wakefulness. This highlights the importance of understanding these molecular processes for better management of the condition.
- Intermittent Hypoxia: Repeated drops in oxygen levels disrupt clock regulation.
- HIF-1 and Clock Genes: Their interaction is crucial for maintaining daily rhythms.
- Altered Feedback Loops: These changes lead to fragmented rest and irregular wakefulness.
By studying these mechanisms, researchers can develop targeted treatments. This knowledge also emphasizes the need for maintaining healthy rest patterns to support the body’s internal clock.
Impact of Intermittent Hypoxia on the Body Clock
Intermittent hypoxia, a hallmark of OSA, plays a significant role in disrupting the body’s internal timing system. This condition involves repeated drops in oxygen levels during rest, which can destabilize the natural rhythms that govern daily functions.
In OSA patients, these oxygen fluctuations stabilize a protein called HIF-1α. This protein is crucial for adapting to low oxygen levels, but its overactivation can alter the expression of clock genes like BMAL1 and CLOCK. These genes are essential for maintaining the body’s daily cycles.
Research Findings on Hypoxia and HIF-1α
Studies have shown that HIF-1α stabilization leads to changes in the circadian system. For example, it can disrupt the feedback loops that regulate the timing of sleep and wakefulness. This misalignment often results in fragmented rest and irregular energy levels.
Key research highlights include:
- Intermittent hypoxia directly affects clock gene expression, leading to misaligned rhythms.
- HIF-1α interacts with BMAL1 and CLOCK, altering their activity patterns.
- These changes can worsen symptoms in OSA patients, making management more challenging.
Understanding these mechanisms is vital for developing targeted treatments. It also underscores the importance of maintaining healthy oxygen levels to support the body’s internal clock. This has significant implications for patient health and overall well-being.
Circadian Rhythm Impact on Sleep Apnea
The connection between internal timing and breathing disruptions is complex yet fascinating. When the body’s daily cycles are misaligned, it can worsen the severity of apnea events. This bidirectional relationship means that disruptions in timing not only trigger apnea but are also exacerbated by it.
Genetic factors play a significant role in this interplay. Certain genes, like BMAL1 and CLOCK, are crucial for maintaining daily rhythms. When these genes are altered, it can lead to both misalignment and apnea. Research shows that individuals with specific genetic markers are more prone to these disruptions.
Recent studies have shed light on this connection. For example, scientists found that hypoxia-inducible factors (HIFs) interact with clock genes, creating a feedback loop. This loop influences the progression of apnea, making it a key area of focus for future treatments.
Here’s a summary of key research findings:
| Research Focus | Findings | Implications |
|---|---|---|
| Genetic Markers | Specific genes linked to both misalignment and apnea. | Helps identify at-risk individuals early. |
| HIF-Clock Gene Interaction | Feedback loops worsen apnea progression. | Targeted therapies can break this cycle. |
| Molecular Mechanisms | Disruptions in clock proteins affect breathing patterns. | Provides insights into disease progression. |
Understanding these mechanisms is essential for developing effective treatments. By addressing both genetic and molecular factors, healthcare providers can offer more personalized care. This approach not only improves symptoms but also enhances overall health.
The Role of the Suprachiasmatic Nucleus and Light-Dark Cycles
The suprachiasmatic nucleus (SCN) acts as the body’s central timekeeper, coordinating daily rhythms. Located in the brain, it collects light cues from the environment to synchronize peripheral clocks. This process, known as entrainment, ensures our biological processes align with the external world.
Entrainment and Master Clock Function
Light-dark cycles are a critical factor in entraining the SCN. When light enters the eyes, it signals the SCN to adjust the body’s internal timing. This synchronization helps maintain a cohesive 24-hour rhythm, essential for overall health.
External light cues also influence gene expression in the SCN. For example, genes like BMAL1 and CLOCK respond to these cues, ensuring the body’s systems function harmoniously. Disruptions in this process can lead to misaligned rhythms and health issues.
Here’s how entrainment works:
- The SCN receives light signals through the eyes.
- It synchronizes peripheral clocks in organs and tissues.
- Gene expression adjusts to maintain daily cycles.
Research highlights the SCN’s role in systemic health. Studies show that a well-functioning SCN supports metabolic and cardiovascular health. Conversely, disruptions can increase the risk of chronic conditions.
| Key Component | Function | Health Impact |
|---|---|---|
| SCN | Master clock coordinating daily rhythms | Supports metabolic and cardiovascular health |
| Light-Dark Cycles | Entrain the SCN and peripheral clocks | Maintains a 24-hour biological rhythm |
| Gene Expression | Adjusts in response to light cues | Ensures harmonious system function |
Understanding the SCN’s role and the importance of light-dark cycles can help improve daily routines. By aligning with natural light patterns, individuals can support their body’s internal clock and enhance overall well-being.
Kinases, Phosphatases, and Their Influence on Clock Function
Enzymes like kinases and phosphatases play a critical role in maintaining the body’s internal timing. These molecules regulate the stability and degradation of clock proteins, ensuring daily biological processes run smoothly. Without their precise activity, the timing system can become disrupted, leading to various health issues.
Phosphorylation, a process driven by kinases, adds phosphate groups to proteins. This modification can either stabilize or mark proteins for degradation. For example, kinases like CK1 and GSK3β target clock proteins such as PER and CRY, influencing their lifespan and activity. On the other hand, phosphatases like PP1 remove phosphate groups, reversing these effects.
Changes in the activity of these enzymes can have significant consequences. When phosphorylation is unbalanced, it can lead to the misregulation of clock proteins. This misregulation often results in disrupted daily cycles, which are linked to conditions like metabolic syndrome. Research shows that altered enzyme activity can contribute to insulin resistance and weight gain, both hallmarks of this condition.
Here’s how kinases and phosphatases influence clock function:
- Kinases (CK1, CK2, GSK3β): Add phosphate groups to clock proteins, affecting their stability.
- Phosphatases (PP1): Remove phosphate groups, reversing kinase effects.
- Impact on Clock Proteins: Changes in phosphorylation alter protein lifespan and activity.
Understanding these mechanisms provides valuable insights into how enzyme activity shapes internal timing. By studying these processes, researchers can develop targeted therapies to address disruptions and improve overall health.
Molecular Interactions: HIF-1α and Clock Genes
The interaction between HIF-1α and clock genes plays a pivotal role in cellular metabolism. HIF-1α, a protein stabilized by low oxygen levels, directly influences the expression of core clock genes like BMAL1 and CLOCK. This molecular interplay helps the body adapt to changing oxygen conditions but can also disrupt daily biological processes when unbalanced.
How Hypoxia Alters Gene Expression
Hypoxia, or low oxygen levels, triggers significant changes in gene expression. When oxygen is scarce, HIF-1α accumulates and binds to DNA, altering the activity of clock genes. This process can lead to shifts in protein production, affecting cellular metabolism and energy regulation.
Here’s how this molecular interaction works:
- HIF-1α Stabilization: Low oxygen levels stabilize HIF-1α, allowing it to interact with DNA.
- Clock Gene Regulation: HIF-1α binds to clock genes, modifying their expression patterns.
- Metabolic Impact: These changes influence protein levels and metabolic pathways.
Research shows that this interaction has broader implications for health. For example, disrupted HIF-1α activity is linked to conditions like cancer, where abnormal cell growth is driven by altered metabolism. Understanding these mechanisms can lead to targeted therapies for metabolic and blood-related disorders.
Key findings include:
- HIF-1α directly regulates the transcription of clock genes, affecting daily rhythms.
- Hypoxia-induced changes in gene expression can lead to metabolic imbalances.
- These molecular shifts are connected to diseases like cancer, highlighting the importance of this research.
By studying the interplay between HIF-1α and clock genes, scientists gain valuable insights into how oxygen levels influence cellular function. This knowledge opens doors to innovative treatments for metabolic and blood-related conditions.
Effects of Sleep Fragmentation on Circadian Regulation
Fragmented rest can throw off the body’s natural timing, leading to widespread health effects. This occurs when rest is repeatedly interrupted, preventing the body from completing its natural cycles. In conditions like OSA, these interruptions are frequent, causing a ripple effect on overall health.
Repeated arousals during rest disrupt the body’s internal clock. This misalignment affects not just rest quality but also the regulation of daily cycles. Over time, these disruptions can lead to systemic issues, impacting various tissues and organ systems.
One of the most affected tissues is the heart. Fragmented rest can strain the cardiovascular system, increasing the risk of hypertension and other heart-related conditions. Studies show that repeated interruptions during rest elevate stress hormones, further taxing the heart.
Here’s how fragmented rest impacts the body:
- Heart Health: Increased stress on the cardiovascular system.
- Metabolic Function: Disrupted cycles can lead to insulin resistance.
- Immune Response: Weakened immune function due to poor rest quality.
Research highlights the systemic consequences of fragmented rest. For example, studies link frequent interruptions to chronic conditions like diabetes and obesity. These findings underscore the importance of addressing rest quality to maintain overall health.
By understanding the effects of fragmented rest, individuals can take steps to improve their daily cycles. This not only enhances rest quality but also supports long-term health and well-being.
Clinical Implications of Circadian Disruption in OSA
Disruptions in the body’s natural timing can lead to serious health complications. In obstructive sleep apnea (OSA), these disruptions are linked to metabolic and cardiovascular issues. Understanding these connections is crucial for effective management and treatment.
Metabolic Consequences
Misaligned timing systems can significantly affect metabolic health. Studies show that OSA patients often experience insulin resistance, a precursor to diabetes. This occurs because disruptions in daily cycles impair glucose regulation.
Research using mouse models has provided valuable insights. For example, altered timing systems in mice led to increased blood sugar levels. These findings highlight the importance of maintaining a healthy daily rhythm to support metabolic function.
Cardiovascular Risks
Cardiovascular health is another area impacted by timing disruptions. Hypertension, or high blood pressure, is a common issue in OSA patients. This occurs because misaligned cycles elevate stress hormones, increasing strain on the heart.
Human studies have shown a clear link between timing misalignment and heart disease. For instance, patients with OSA often have higher blood pressure levels during sleep. Addressing these disruptions can help reduce cardiovascular risks.
| Health Risk | Description | Evidence |
|---|---|---|
| Insulin Resistance | Impaired glucose regulation leading to diabetes risk. | Mouse studies show elevated blood sugar levels. |
| Hypertension | High blood pressure due to elevated stress hormones. | Human research links OSA to increased blood pressure. |
| Heart Disease | Increased strain on the heart from misaligned cycles. | Studies show higher cardiovascular risks in OSA patients. |
By understanding these clinical implications, healthcare providers can offer more targeted treatments. Addressing timing disruptions not only improves OSA symptoms but also supports overall health.
Linking Circadian Misalignment to Diabetes and Obesity
Misaligned daily cycles can lead to significant health challenges, particularly in metabolism. When the body’s internal timing is disrupted, it can trigger a cascade of issues, including insulin resistance, diabetes, and obesity. Understanding this connection is key to addressing these conditions effectively.
Insulin resistance often develops when the body’s natural timing is off. This occurs because misalignment affects the release of hormones that regulate glucose metabolism. Over time, this can lead to higher blood sugar levels and an increased risk of diabetes.

Insights into Insulin Resistance
Insulin resistance is a condition where the body’s cells don’t respond well to insulin, a hormone that helps regulate blood sugar. When daily cycles are misaligned, the timing of insulin release can be disrupted. This makes it harder for the body to process glucose efficiently.
Hormonal changes during the day play a significant role in this process. For example, cortisol levels naturally rise in the morning to help wake the body. If this rhythm is disrupted, it can lead to imbalances that affect insulin sensitivity.
Recent studies have shown a clear link between timing misalignment and metabolic disorders. For instance, research on shift workers found that irregular schedules increase the risk of diabetes and obesity. These findings highlight the importance of maintaining a consistent daily routine.
| Mechanism | Effect on Metabolism | Health Outcome |
|---|---|---|
| Hormonal Imbalance | Disrupted insulin release | Increased blood sugar levels |
| Glucose Regulation | Reduced insulin sensitivity | Higher risk of diabetes |
| Energy Storage | Altered fat metabolism | Increased risk of obesity |
By understanding these mechanisms, we can better address the root causes of metabolic disorders. Maintaining a healthy daily rhythm is essential for supporting overall health and preventing these conditions.
Tissue-Specific Transcriptomic Changes from Intermittent Hypoxia
Gene expression patterns shift dramatically under intermittent hypoxia conditions. This phenomenon affects various tissues, including the lung, heart, and liver. Understanding these changes can provide valuable insights into how hypoxia influences health.
Animal models have been instrumental in studying these effects. Mice exposed to intermittent hypoxia show significant alterations in gene expression across different organ systems. These findings highlight the complex relationship between hypoxia and tissue function.
Animal Models and Research Highlights
Research using mice has revealed key changes in the lung and heart. For example, hypoxia disrupts the expression of genes involved in oxygen transport and energy production. These disruptions can lead to long-term health issues if left unaddressed.
Studies also show that gene expression patterns vary across tissues. While the lung may respond by increasing inflammation-related genes, the heart might focus on stress response mechanisms. This tissue-specific variability underscores the complexity of hypoxia’s effects.
Key research highlights include:
- Lung tissue shows increased expression of genes linked to inflammation and fibrosis.
- Heart tissue experiences changes in genes related to energy metabolism and stress response.
- Liver tissue exhibits altered expression of genes involved in detoxification and metabolism.
These findings illustrate how hypoxia impacts different organ systems. By understanding these changes, researchers can better address the development of hypoxia-related diseases.
The implications of these findings are far-reaching. They not only shed light on the mechanisms of hypoxia but also open doors to targeted therapies. By focusing on tissue-specific responses, healthcare providers can offer more personalized treatments.
Implications for Future Research and Therapeutic Approaches
Exploring new research directions can unlock innovative treatments for complex health conditions. By focusing on the molecular interplay between hypoxia and internal timing, scientists are paving the way for breakthroughs in managing related complications. This understanding can lead to therapies that reduce risk and improve overall health outcomes.
One promising avenue is the development of compounds that reset the body’s natural timing. These therapies aim to address disruptions at the molecular level, offering a targeted approach to treatment. For example, researchers are investigating small molecules that can stabilize clock proteins, restoring balance to daily cycles.
Another focus is on validating preliminary findings through large-scale studies. These efforts will help confirm the effectiveness of emerging therapies and refine their application. By combining clinical trials with advanced molecular analysis, researchers can ensure that new treatments deliver the desired result.
Here’s a summary of emerging therapeutic strategies:
| Strategy | Description | Potential Impact |
|---|---|---|
| Small Molecule Therapies | Compounds that stabilize clock proteins. | Restores natural timing, reduces risk of complications. |
| Gene Editing Techniques | Targets specific genes to correct disruptions. | Offers long-term solutions for health management. |
| Light-Based Therapies | Uses light exposure to reset internal timing. | Non-invasive approach with minimal side effects. |
Future research will also explore the broader implications of these therapies. For instance, understanding how they affect other health conditions can expand their application. By addressing the root causes of disruptions, these treatments have the potential to transform health care.
As the field advances, collaboration between researchers and clinicians will be crucial. Together, they can translate scientific discoveries into practical solutions, improving the lives of those affected by these conditions. The future of health management looks promising, with innovative therapies on the horizon.
Practical Tips for Managing Sleep Apnea and Resetting Your Body Clock
Managing sleep apnea effectively requires a combination of lifestyle changes and expert guidance. By making small adjustments to your daily routine and following expert recommendations, you can improve your sleep quality and align your body clock for better health.
Daily Routine Adjustments
Consistency is key when it comes to resetting your body clock. Start by setting a regular sleep schedule. Go to bed and wake up at the same time every day, even on weekends. This helps your body establish a natural rhythm.
Physical activity also plays a crucial role. Aim for at least 30 minutes of moderate exercise daily. Activities like walking, yoga, or swimming can improve sleep quality and reduce apnea symptoms.
Dietary habits matter too. Avoid heavy meals, caffeine, and alcohol close to bedtime. Instead, opt for light snacks like a banana or a handful of nuts to promote better rest.
Expert Recommendations for Better Sleep
Experts suggest creating a sleep-friendly environment. Keep your bedroom cool, dark, and quiet. Use blackout curtains and white noise machines if needed. These small changes can make a big difference.
Light exposure management is another important factor. Spend time outdoors during the day to soak up natural light. In the evening, reduce exposure to screens and bright lights to signal your body that it’s time to wind down.
Consider consulting a sleep specialist for personalized advice. They can recommend therapies like CPAP machines or oral appliances to help control apnea symptoms.
| Tip | Description | Benefit |
|---|---|---|
| Set a Sleep Schedule | Go to bed and wake up at the same time daily. | Helps establish a natural rhythm. |
| Exercise Regularly | Engage in 30 minutes of moderate activity daily. | Improves sleep quality and reduces symptoms. |
| Optimize Your Environment | Keep your bedroom cool, dark, and quiet. | Promotes better rest and relaxation. |
By incorporating these practical tips into your routine, you can take control of your sleep apnea and support your body’s natural timing. Small changes can lead to significant improvements in your overall health and well-being.
Wrapping Up Insights on the Sleep Apnea and Circadian Clock Connection
Understanding the link between internal timing and breathing disruptions offers new hope for managing related syndromes. This connection highlights how hypoxia and misaligned cycles contribute to health challenges, emphasizing the need for integrated care approaches.
Research continues to uncover the complex relationship between these factors, paving the way for innovative treatments. By addressing disruptions at their root, we can improve overall well-being and reduce the risk of complications.
Further exploration of these mechanisms is essential. If you’re experiencing symptoms, consider consulting a healthcare professional for personalized advice. Together, we can work toward better health and quality of life.

